In the eyes of many, nursing home care is an inevitable transition older adults must make as they age. But in New York, several programs are aimed at helping older adults, families, and those with disabilities live independently.
Millions of Americans rely on medical equipment, health services, and treatments covered by Medicaid; home care services are no exception. But to what extent does Medicaid cover home care services, and how can you ensure you receive the financial support you need to live at home?
Below, we delve into the details you need to know to get the assistance you deserve.
Key Takeaways
- Medicaid can cover in-home care in New York for those who meet certain eligibility requirements.
- Depending on the level of care a beneficiary needs, different supportive services — including home health aides, compensation for family caregivers, and more — may be covered.
- Talk to your doctor to learn if you qualify for Medicaid-covered home health care services and your options for care.
Apply for CDPAP or HHA today
Does Medicaid Pay for In-Home Care in New York?
Medicaid in New York can pay for in-home care services for eligible individuals. In fact, many Medicaid-funded Home Care programs are designed to help older adults or individuals with disabilities live safely at home rather than in a nursing home.
In New York, different home health care programs come with unique eligibility requirements. However, they all require that a person be eligible for Medicaid to participate.
With the right information handy, beneficiaries can demonstrate their medical needs and receive financial support that helps them live safely and comfortably in their own homes.
New York Home Care Services Program
The New York Home Care Services Program features various long-term care programs that aim to help eligible individuals maintain their independence and remain safely at home. Since Medicaid covers these programs, they have specific eligibility requirements and general limitations.
Options for Long-Term Care
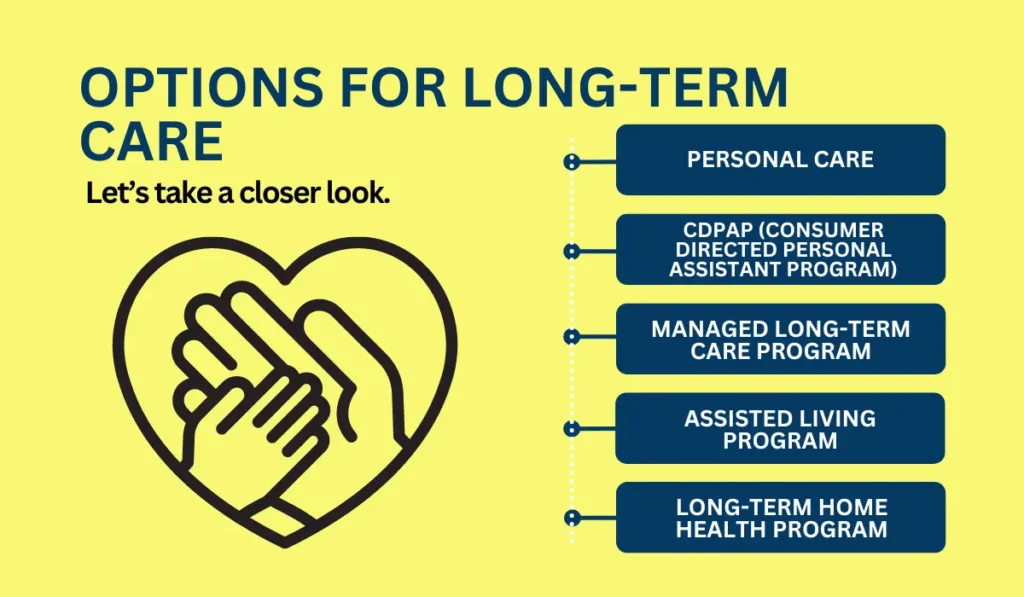
The long-term care options within New York’s Home Care Services Program vary in terms of what they cover and who an ideal candidate might be. Let’s take a closer look.
- Personal Care: Also referred to as Medicaid-funded home care, personal care involves using home attendant and housekeeping services for those who face challenges with one or more activities of daily living (ADLs). Examples of ADLs might include personal hygiene, nutrition, and more. Individuals who choose this option must be Medicaid eligible and otherwise exempt from managed long-term care.
- CDPAP (Consumer Directed Personal Assistant Program): This program is another option for personal care services. CDPAP allows participants to choose their own caregivers (such as family members, friends, and other loved ones) who can receive compensation for their work. It allows consumers to take control of their care while receiving the financial and other assistance they need.
- Managed Long-Term Care Program: This program covers a wide range of home care services, including case management, nursing, home health aides, physical therapy, and home attendant services for those who are Medicaid eligible. Individuals eligible for both Medicaid and Medicare can also take advantage of this program.
- Assisted Living Program: Through adult care facilities (ACFs), this program offers long-term, non-medical residential services to individuals who cannot live alone due to physical, mental, or other limitations. To qualify for assisted living programs, individuals must not need continued medical care or nursing services in other health facilities (like nursing homes or hospitals) because ACFs are not licensed to provide such support.
- Long-Term Home Health Program: Individuals participating in this program must create a plan of medical, nursing, and rehabilitative care to be provided at home. Those who use this program must be medically eligible for placement in a nursing home but have care costs that are lower than the nursing home cost near them.
Who Is Eligible for Medicaid In-Home Care?
Eligibility requirements for Medicaid in-home care depend on where a person applies for coverage. Different eligibility categories come with their own requirements and exceptions.
However, many Medicaid applications go to the NY State of Health, which determines eligibility using a person’s Modified Adjusted Gross Income (MAGI).
This essentially means that federal tax income information is used to determine eligibility. But other factors can influence eligibility when combined with an applicant’s MAGI, including:
- Age
- Disability status
- Pregnancy status
- Household size
MAGI rules use the federal poverty level (FPL) as a guide for eligibility to ensure that low-income applicants receive the support they need. As a result, income limits for individuals who qualify for Medicaid through MAGI rules are as follows:
| Pregnant consumers | 223% FPL |
| Children under 1 | 223% FPL |
| Children ages 1 through 5 | 154% FPL |
| Children ages 6 through 18 | 110% – 154% FPL |
| Parents, caretakers, and relatives | 138% FPL |
| 19 and 20-year-olds living with parents | 138% – 155% FPL |
| Single/childless couples and 19 and 20-year-olds living alone | 100% – 138% FPL |
| Family planning program | 223% FPL |
Medicaid coverage is also available for individuals not part of MAGI eligibility groups. These applicants, who are part of what’s known as non-MAGI eligibility groups, must apply for coverage with their Local Department of Social Services or a Facilitated Enroller for the Aged, Blind, and Disabled.
Examples of non-MAGI eligibility groups include:
- Adults 65 years of age or older who are not a parent or caretaker relative
- Individuals who are blind or disabled and do not meet MAGI eligibility criteria
- Residents of Adult Homes run by residential care centers, community residences, LDSS, etc.
- Individuals who are eligible for other health coverage programs, including the Medicare Savings Program (MSP), COBRA, Aids Health Insurance Program, and Medicaid Buy-in Program for Working People with Disabilities
- Individuals formerly or currently in foster care
Beyond these specific criteria, other factors that might impact a person’s Medicaid eligibility status include:
- State of residency
- Citizenship or immigration status
Beneficiaries who qualify for the Medicaid program can receive home care services based on their established needs and ideal treatment approach. An individual’s level of independence and the cost of their care influence which medical services and home care programs are the best fit.
What Is the Process to Receive Medicaid In-Home Care?
To receive Medicaid coverage for in-home care, it’s necessary to first ensure you qualify for Medicaid. From there, you can move forward with visiting a medical professional for an official assessment.
Your provider can determine whether you’re eligible for a particular home care program and sign appropriate paperwork to verify you meet the requirements to qualify.
Depending on the type of home care services you seek (particularly the CDPAP program), you may also need to partner with a fiscal intermediary to gain access to social services that will help you manage wages and other financial benefits.
You might also need to work with your care provider to create a specific care plan you’ll use.
Once your application is submitted to the appropriate office or agency, it’s processed, approved, or denied. Those who successfully enroll in a home care program can then make arrangements to receive the services they need.
Remember, different home care services may come with specific steps and requirements you need to follow to receive coverage. Still, popular options like the CDPAP program are fairly straightforward; working with your doctor throughout the application process can simplify things even further.
Overall, you can expect Medicaid to pay for home care services as long as you prove you qualify and meet the right criteria for each program. Medicaid coverage enables beneficiaries from all walks of life to find the support they need to live independently and safely.
Don’t hesitate to see if you can take advantage of its benefits as you develop a long-term care plan that works for you.