If you’re approved for Medicaid in New York, you’ll receive a Common Benefit Identification Card, also called a Medicaid card. This ID card is your proof of enrollment in the Medicaid program.
But what your Medicaid card looks like and how it works can vary based on your plan and eligibility. Here’s what your card might look like, how to use it, and why it matters more than you might think.
Key Takeaways
- Medicaid cards in New York can look different based on your plan, care setting, or enrollment type.
- The CBIC is the standard Medicaid ID card, while managed care plans give you their insurance card.
- A lost or damaged Medicaid card can be replaced or temporarily issued by visiting a Medicaid office in person.
- Friends & Family offers help with Medicaid-covered home care and support for questions about eligibility and services.
What Your Medicaid Card Looks Like in New York
Depending on how you get your Medicaid coverage, your card might look a little different. Here’s what you need to know about the types of cards you might have, and what each one means when you go to get care:
The Standard CBIC Medicaid Card
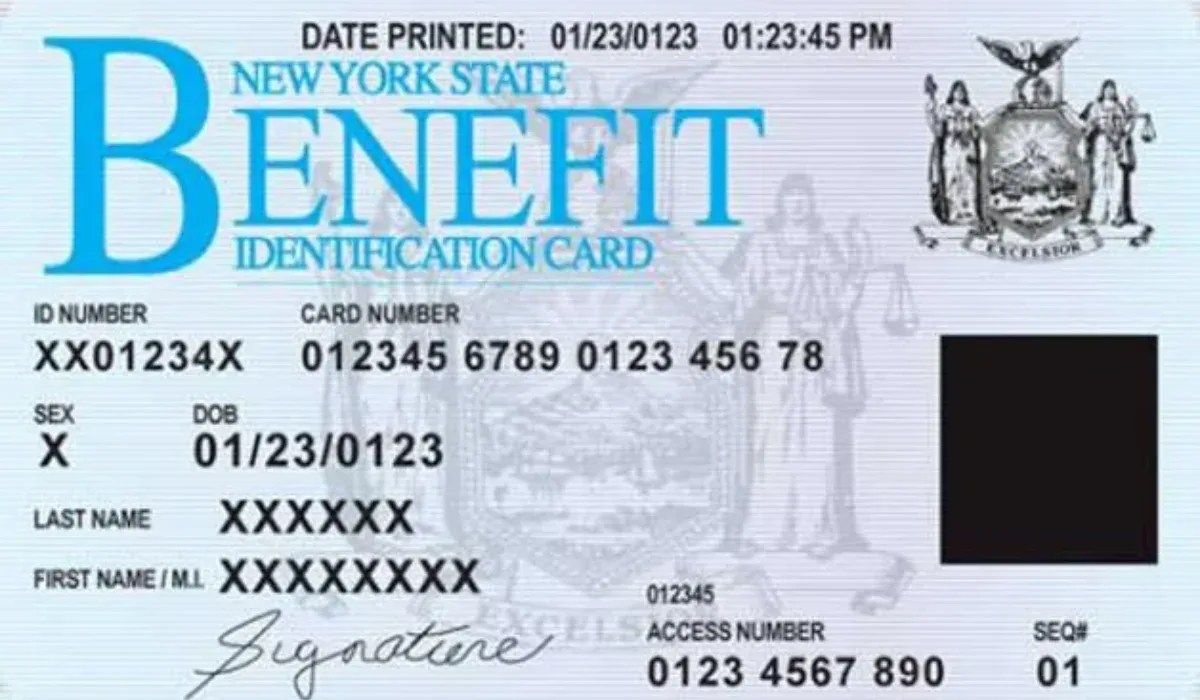
The Common Benefit Identification Card (CBIC) is a plastic ID card issued by the New York State Department of Health. It includes your name, a Medicaid ID number (also known as a CIN), and the date of issue. There’s a magnetic stripe on the back, and the words “Benefit Identification Card” are printed clearly at the top.
This is the default card for those in fee-for-service Medicaid.
You’ll use this card with most health care providers in New York who accept Medicaid. It’s part of your health care coverage and connects you directly to Medicaid services without going through a separate health plan.
Managed Care Health Plan Cards
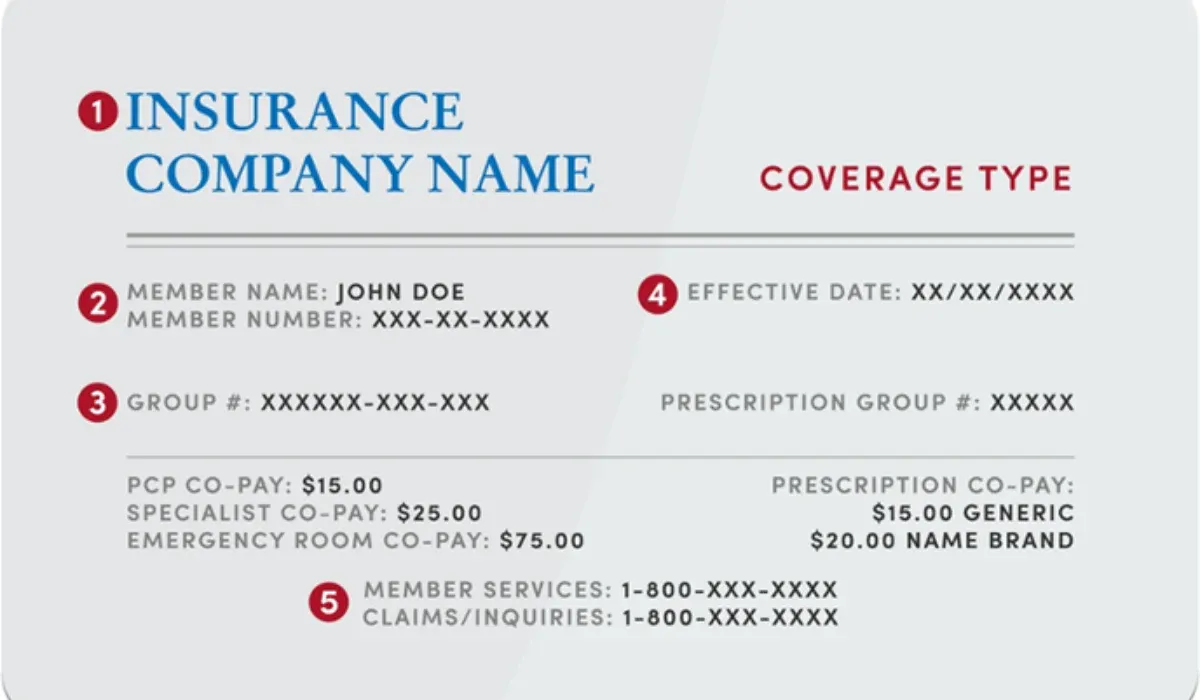
If you’re part of a managed care plan, such as one from Healthfirst, MetroPlus, or Fidelis, you’ll receive a health insurance card from that provider instead. This card will look more like a private insurance ID card, with your name, member ID, contact information, and sometimes the name of your primary Medicaid provider.
Your managed care plan helps coordinate your medical care. That includes preventive services, mental health care, and hospital stays. These cards ensure that your health care providers know where to send the bill.
Replacement Cards and Temporary ID Cards
If your card is lost, stolen, or damaged, don’t worry. You can request a new card by calling the Medicaid Helpline. It’s a toll-free hotline at (888) 692-6116. You’ll need to provide your date of birth and social security number. The department will verify your Medicaid eligibility and mail you a replacement card to the address on file.
If you need to be seen by a provider before your new card arrives, you may be able to get a temporary ID card by visiting a Medicaid office in person. Bring a government-issued ID, like a driver’s license, and ask for help at the front desk.
Medicaid Cards for Foster Care or Institutional Care
Children in foster care or people living in facilities often have Medicaid cards that are managed by a guardian, care coordinator, or staff. These cards include the Medicaid ID number and all necessary info, but are often stored for safekeeping and used by the facility when arranging appointments or accessing care.
This system helps those with disabilities or mental health needs get consistent care, even if they can’t manage their documents.
Why Your Medicaid Card Matters
Your Medicaid card is more than an ID. It’s your key to accessing essential health care services. Here’s why it matters to every Medicaid member:
It Confirms Your Enrollment and Eligibility
When you go to a medical appointment or pick up medicine, your card proves that you’re a current Medicaid beneficiary. Health care providers use it to check your eligibility and make sure you’re covered.
Without the right ID card, you may be turned away or asked to pay for medical services upfront.
It Prevents Billing Mistakes and Co-payments
Most Medicaid members don’t have to pay out of pocket. Over 7.5 million New Yorkers are enrolled in Medicaid, making it one of the largest public insurance programs in the state. But if a provider can’t verify your Medicaid coverage, they may bill you or charge co-payments you don’t owe.
Presenting your card ensures that medical services are billed correctly to the Medicaid program or your managed care health plan.
It Tells Providers Where to Send Bills
The Medicaid card also directs providers to the correct billing office, whether it’s the state or your specific managed care plan. This helps avoid payment delays and ensures you get continuous care.
For example, if you’re in a Medicare-Medicaid plan, your providers may need to coordinate services through both systems.
It Helps You Get the Care You Need, Faster
Having the right ID number and up-to-date information on your card helps speed up appointments and pharmacy visits. It also links to your full health care history, including past visits, prescription details, and approved services.
This makes it easier to get follow-up care or referrals, especially for complex needs like home care or long-term support.
Need Help With Your Medicaid Card or Medical Care?
At Friends & Family Home Care, we work with New York residents every day who rely on Medicaid for essential health care services. While we don’t issue Medicaid cards directly, we can point you to the right steps if you’ve lost your card or need help understanding your Medicaid benefits.
We also provide traditional home care options through certified HHAs and PCAs.
If you’re looking for guidance on getting started or continuing with your Medicaid-covered home care, reach out to us.