If you’re on Medicaid and need foot care, you might wonder what’s covered. Foot problems like bunions, corns, or diabetic foot issues are uncomfortable and can lead to serious health risks if untreated.
Fortunately, Medicaid in New York provides coverage for many podiatry services. However, the specifics can vary depending on your plan and eligibility.
In this post, we’ll break down what Medicaid covers, how to check your coverage, and what to do if your care isn’t included. Whether dealing with routine foot care or more complex podiatric conditions, we’ll guide you through finding the right options for your needs.
Key Takeaways
- Medicaid in New York covers routine foot care, diabetic foot treatment, and deformity corrections, often requiring prior authorization or referrals.
- Review your plan, contact Medicaid, or consult healthcare providers to confirm podiatry coverage.
- Explore sliding-scale clinics, alternative insurance, or other payment options if Medicaid doesn’t cover your care.
- Use directories, health plans, or referrals to find Medicaid-accepting podiatrists in NYC.
What Foot Care Does Medicaid Cover?
Medicaid in New York provides coverage for many podiatry services. Mostly, it focuses on treatments that address medical conditions or prevent serious complications. Routine foot care, such as trimming toenails or treating corns and calluses, is often included when deemed medically necessary.
This is particularly important for individuals with diabetes or disabilities who are at higher risk for infections or other complications.
Diabetic Foot Care
For those managing diabetes, Medicaid covers essential services like foot exams, ulcer treatments, and preventive care to reduce the risk of severe outcomes, such as infections or amputations.
Medicaid also provides coverage for podiatric procedures to correct deformities like bunions and hammertoes, though these often require documentation proving medical necessity.
Requirements for Coverage
Some services might come with additional steps, such as prior authorization. This means Medicaid needs to approve the treatment in advance to confirm it aligns with their guidelines.
Referrals from a primary care doctor are also commonly required, especially for services provided in nursing facilities or outpatient clinics.
In general, coverage details can vary depending on your plan. Fee-for-service plans and managed care options might have different rules or networks for podiatric care. To avoid unexpected costs, it’s always a good idea to check with your provider or the New York State Medicaid program before scheduling an appointment.
How to Determine If Your Coverage Includes Podiatry
Understanding your Medicaid coverage for podiatry services can save time and prevent unexpected costs. Coverage specifics often depend on your Medicaid plan and the type of care you need. Here’s how to check:
Review Your Medicaid Plan
Start by reviewing your plan details. If you’re enrolled in a managed care plan, check the list of covered services provided by your insurer.
Look for specific podiatry services like routine foot care, treatment for diabetic foot conditions, or coverage for deformities such as bunions and hammertoes.
Contact the New York State Medicaid Program
For questions about what Medicaid covers in New York, reach out to the New York State Department of Health (NYSDOH). Their resources can clarify general eligibility, referral requirements, and any prior authorization rules for podiatric care.
Lastly, your primary care doctor or podiatrist’s office can often verify coverage for specific services. They can check procedure codes and confirm whether your plan requires a referral or pre-approval for the treatment.
What to Do If Medicaid Doesn’t Cover Your Care
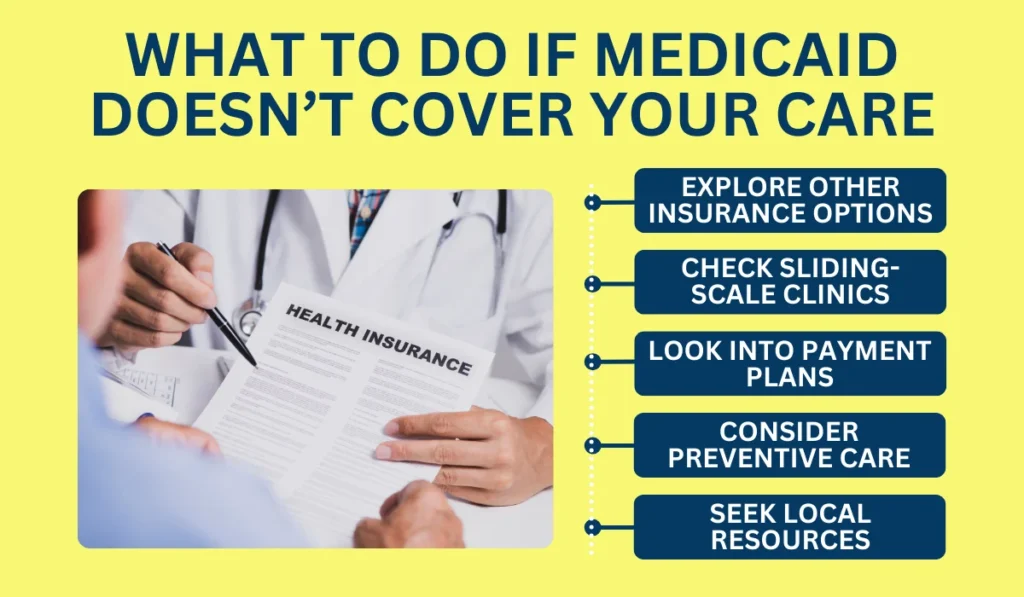
If Medicaid doesn’t cover the podiatry services you need, there are still ways to access the care you require. Here are practical options to consider:
- Explore Other Insurance Options: Check if you qualify for programs like Medicare. Dual-eligibility plans often expand podiatry coverage for routine and specialized care.
- Check Sliding-Scale Clinics: Many clinics in New York adjust costs based on income, offering affordable care for bunions, diabetic foot issues, or orthotics.
- Look into Payment Plans: Some podiatry offices provide financing options, letting you spread out costs for uncovered services.
- Consider Preventive Care: Maintain good foot hygiene, wear proper footwear, and address minor issues early to avoid serious problems.
- Seek Local Resources: Nonprofits or community groups in NYC may offer grants or subsidies for podiatry services.
Luckily, even if Medicaid doesn’t cover your care, these strategies can help you find affordable solutions while managing your foot health effectively. Taking proactive steps ensures you get the care you need without unnecessary stress.
How to Find a Podiatrist That Accepts Medicaid in NYC
Finding a podiatrist who accepts Medicaid in New York City doesn’t have to be complicated. Here are a few ways to simplify your search:
Start with Medicaid and Your Health Plan
Use the New York State Medicaid program’s online provider directory to find podiatrists who accept Medicaid. This tool allows you to search by location, specialty, or other filters.
If you’re on a managed care plan, check their website or contact customer service for a list of in-network providers.
Use Local Clinics and Referrals
Many podiatry clinics in NYC, Brooklyn, and Manhattan accept Medicaid patients. Call local offices to confirm participation and learn about documentation or referral requirements.
Your primary care doctor can also recommend podiatrists who accept Medicaid and assist with obtaining referrals or prior authorization if needed.
Focus on Specialized Services When Necessary
If you need care for specific conditions, such as diabetic foot issues, orthotics, or deformities, look for podiatrists who specialize in these areas. Use online directories or contact clinics directly to verify their expertise and Medicaid acceptance.
Alternatively, you can let professional home care services point you in the right direction. It’ll save you time and headache so you can manage your or your loved one’s feet’ health more conveniently.